Definition and Causes:
DEFINITION: This is a chronic inflammatory joint disease involving progressive loss of joint cartilage. There are over 100 different types of arthritis; most common among these are osteoarthritis and rheumatoid arthritis. CAUSES: Osteoarthritis can be divided into:
- Primary Osteoarthritis: Results due to regular wear and tear of the joint cartilage. As we age, the water content of the cartilage increases; while the protein content degenerates, resulting in weak and flaky cartilage
- Over time, this gradual degeneration of the cartilage, continuous use of affected joint, causes further degeneration and inflammation with pain. Eventually, leads to bone/joint deformity (overgrowth) and decreased mobility
- Secondary Osteoarthritis: Caused by some other disease or condition e.g. obesity, repeated trauma or surgery of the joints, congenital joint abnormalities, gout, and hormonal disturbances like diabetes or growth hormone disorders
Symptoms:
Pain is the main symptom associated with OA, which is typically exacerbated by repetitive use of the affected joints, and relieved by rest. Symptoms are variable from patient to patient but often include:
- Morning stiffness always <20-30 minutes
- Crepitations may be noted with the movement of the joint.
- Joint involvement progresses slowly and irreversibly
- Some patients with osteoarthritis of the finger and knee may have years of pain-free interval between symptoms
- Arthritis of the knees is often associated with excess upper body weight
- Can affect the spine and cause neck (cervical) or low back (lumbar) pain
- Bone spurs, called osteophytes that form along the bones of the spine can irritate spinal nerves, causing severe pain that can radiate from the spine as well as numbness and tingling of the affected parts of the body, e.g. sciatica (pain radiating from the low back through the buttock into the leg)
- Osteoarthritis causes the formation of hard, bony enlargements of the small joints of the fingers. The swollen enlarged joints at the ends of the fingers are sometimes called a Heberden’s node. The presence of these nodes can be helpful in diagnosing osteoarthritis
Investigations and Treatment:
INVESTIGATION:
Laboratory: There is no blood test for the diagnosis of osteoarthritis. However, the blood test may be obtained to:
- Exclude other arthritic conditions (e.g. rheumatoid arthritis) or other conditions that might cause joint inflammation (e.g. gout or infections)
- Monitor disease status and response to treatment
- Monitor medication effects
X-rays: Common findings related to the affected joints may include:
- Loss of joint cartilage
- Narrowing of the joint space between adjacent bones
- Bone spurs formation
- Helpful to exclude other causes of pain in a particular joint and assists in making a decision, as to when surgical intervention might be considered
Arthroscopy:
- A procedure that involves the insertion of a viewing tube into the joint space. Abnormalities/damage to the cartilage and ligaments can be seen and repaired sometimes through the arthroscope. It is very helpful in making the definitive diagnosis of osteoarthritis
Arthrocentesis: A minor procedure to remove fluid from the joint through a sterile needle. This procedure can be used to:
- Analyze for gout, infection, and other causes of arthritis
- Instill corticosteroids into the joints to help relieve pain, swelling, and inflammation
TREATMENT: Treatment of OA revolves around the minimization of symptoms (i.e. reduce joint pain, inflammation, improve mobility) and maintenance of the quality of life. Some patients may have minimal or no pain and do not require medications. A small percentage of patients may benefit from conservative lifestyle changes such as:
- Rest
- Exercise
- Weight loss
- Diet improvement (to include more vitamins)
- Physiotherapy/ occupational therapy
- Mechanical support devices (e.g. knee braces)
These measures are particularly helpful when large joints are involved. Medications are used to complement the above measures. Topical, oral or injectable medications are recommended as needed.
Most commonly used medications are as follows:
Mild pain reliever:
- Aspirin and acetaminophen (Tylenol, Vicodin, Percocet)
- Anti-inflammatory (Advil, Motrin)
Pain-relieving creams:
- Capsaicin (ArthriCare, Zostrix), salycin (Aspercreme), methyl salicylate (Ben-Gay, Icy Hot), and menthol (Flexall)
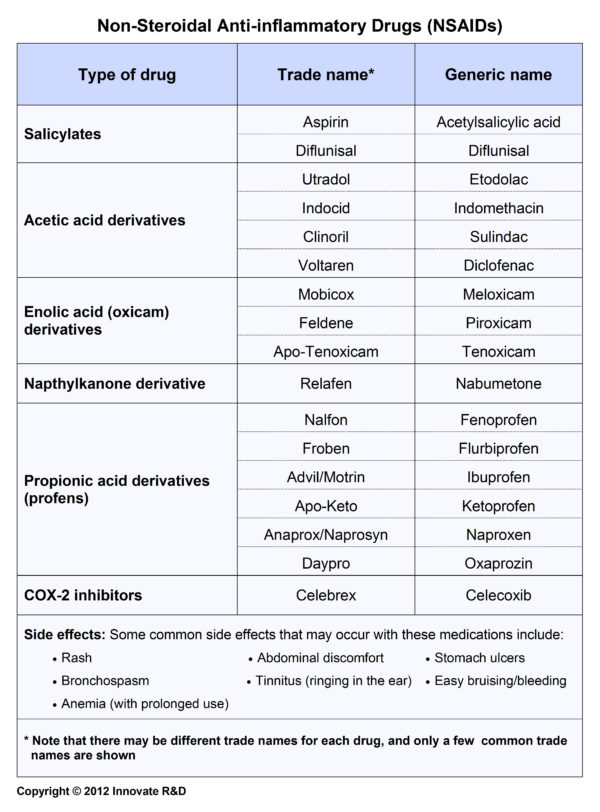
- Nonsteroidal anti-inflammatory drugs (NSAIDs): ibuprofen (Motrin), nabumetone (Relafen), and naproxen (Naprosyn)
Oral analgesics for mild pain:
Non-NSAID analgesic:
- Acetaminophen (Tylenol, Vicodin, Percocet)
Topical analgesic agents:

Persistent pain in severe osteoarthritis:
- Corticosteroid injections directly into the inflamed joints benefit and rapidly decrease pain
- Hyaluronic acid (Synvisc, Hyalgan, Orthovisc, Supartz, and Euflexa) injections into the joint can sometimes be helpful, especially if surgery is not being considered
Pain-relieving injections:

NOTE: While there are potential side effects from using these medications, there are also the effects of untreated OA – which includes increase pain and joint damage with disease progression leading to decreasing mobility and overall poor quality of life. Consequently, the treating physician will assess the side effect risks versus the benefits in controlling symptoms and improving quality of life (risk versus benefit ratio), before recommending treatment. If the patient has other medical conditions or using other medications, these are taken into account when prescribing medications. The patient is advised to take note of and report potential side effects to the treating physician.
Surgery: Generally reserved for patients, who are unresponsive to the other treatments with severe osteoarthritis.
Joint replacement surgery:
- This procedure is reserved for unresponsive patients to improve their condition. During surgery, patients are usually anesthetized (put to sleep), and the damaged joint is removed and replaced with an artificial one. Hips and knees are the most often replaced joints. Patients may take months of rehabilitation to strengthen the joint
Risk Factors and Prevention:
Risk Factor Management
- Obesity
- Inactive lifestyle
- Family history of the disease
- Age – more common in individuals over 65
- Joint trauma
- Diet
- Certain types of infection
To reduce the risk of arthritis patients should:
- Maintain a healthy weight
- Exercise regularly
- Wear appropriate equipment to minimize injury during sport
- Adopt appropriate measures, to minimize sport injury
- Ensure diet contains necessary vitamins and minerals
Outcome:
- OA is incurable. Early diagnosis and treatment may help to reduce or delay joint injury
- Chronic cases will require lifelong treatment
- Early recognition and lifestyle modification may help improve quality of life








